Between 1 January to 10 July 2022, a cumulative number of 7796 cases of Cholera including 37 associated deaths (a case fatality ratio of 0.5%) have been reported from 25 drought-affected districts, according to a press release issued by the World Health Organization on 20 July 2022. Cholera is endemic in Somalia with recurrent outbreaks reported since 2017.
The current Cholera outbreak is taking place in the context of other ongoing outbreaks, high rates of malnutrition, and the escalating drought, all of which are exacerbating the fragility of Somalia’s humanitarian situation and have led to large displacement of people, placing additional pressure on an already over-burdened and underperforming healthcare system. Currently, the country has limited capacity to respond to the outbreak, increasing the risk of serious public health impact.
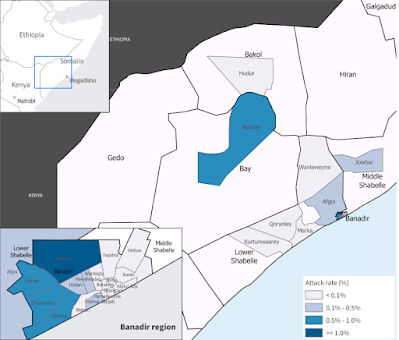
From 1 January to 10 July 2022, according to the Ministry of Health Somalia, a cumulative number of 7796 cases of cholera including 37 associated deaths have been reported from 25 drought-affected districts in Banadir region, South-West State and Hirshabelle State. The districts reporting the highest number of cases include Baidoa (2033), Daynile (1080), Jowhar (825) and Afgoi (681). In addition to being the drought-affected districts, many of these districts also host Internally Displaced Populations in camps resulting from three decades of conflict and the escalating drought situation.
Over half of the cases (53.5%) were among children below two years of age, with males and females equally affected. Severe dehydration was reported in 27% of cases. None of the cases reported having received .Oral Cholera Vaccine Oral Cholera Vaccine campaigns were carried out in Somalia in 2017, 2018 and 2019.
As of 10 July, a total of 677 stool samples were collected and analysed (by culture) by the National Public Health Laboratory in Mogadishu. Of these, 145 samples (21.4%) tested positive for Vibrio cholerae.
The number of cases reported in the first six months of 2022 has exceeded the number of cases reported in 2021 in the same drought affected districts, when a total of 6205 acute watery diarrhoea/suspected cholera cases including 39 deaths (a case fatality ratio of 0.63%) were reported. In 2021, the outbreak started following flash floods.
Cholera is an acute enteric infection caused by ingesting the Bacterium Vibrio cholerae, a Gram-negative, comma-shaped Gammaproteobacteria, related to other pathogenic Bacteria such as Yersinia pestis (Bubonic Plague), and Esherchia coli (food poisoning), which present in contaminated water or food. It is mainly linked to insufficient access to safe drinking water and inadequate sanitation. It is an extremely virulent disease that can cause severe acute watery diarrhoea resulting in high morbidity and mortality, and can spread rapidly, depending on the frequency of exposure, the exposed population and the setting. Cholera affects both children and adults and can be fatal if untreated.
The incubation period is between 12 hours and five days after ingestion of contaminated food or water. Most people infected with Vibrio cholerae do not develop any symptoms, although the Bacteria are present in their faeces for 1-10 days after infection and are shed back into the environment, potentially infecting other people. Among people who develop symptoms, the majority have mild or moderate symptoms, while a minority develop acute watery diarrhoea with severe dehydration. Cholera is an easily treatable disease. Most people can be treated successfully through prompt administration of oral rehydration solution.
Cholera can be endemic or epidemic. A Cholera-endemic area is an area where confirmed Cholera cases were detected during the last three years with evidence of local transmission (cases are not imported from elsewhere). A Cholera epidemic can occur in both endemic countries and in non-endemic countries. Uninfected dead bodies have never been reported as the source of epidemics.
The consequences of a humanitarian crisis – such as disruption of water and sanitation systems, or the displacement of populations to inadequate and overcrowded camps – can increase the risk of Cholera transmission, should the bacteria be present or introduced.
A multisectoral approach including a combination of surveillance, improving access to clean water, sanitation, and hygiene promotion, rapid access to treatment, risk communication and community engagement and oral cholera vaccines is essential to control cholera outbreaks and to reduce deaths.
Follow Sciency Thoughts on Facebook.
Follow Sciency Thoughts on Twitter.